Do you enjoy consuming chocolate, mint, or caffeine? Who doesn’t! While they may be tasty, they might be causing you heartburn, regurgitation and indigestion if regularly overindulged. If you have experienced one or more of these symptoms then you could be diagnosed with GERD (Gastroesophageal Reflux Disease), or the malfunction of your sphincter. When this occurs, gastric acid flows back into your esophagus causing irritation and damage to the esophageal lining (5).
What is Gastroesophageal Reflux Disease ( GERD )?
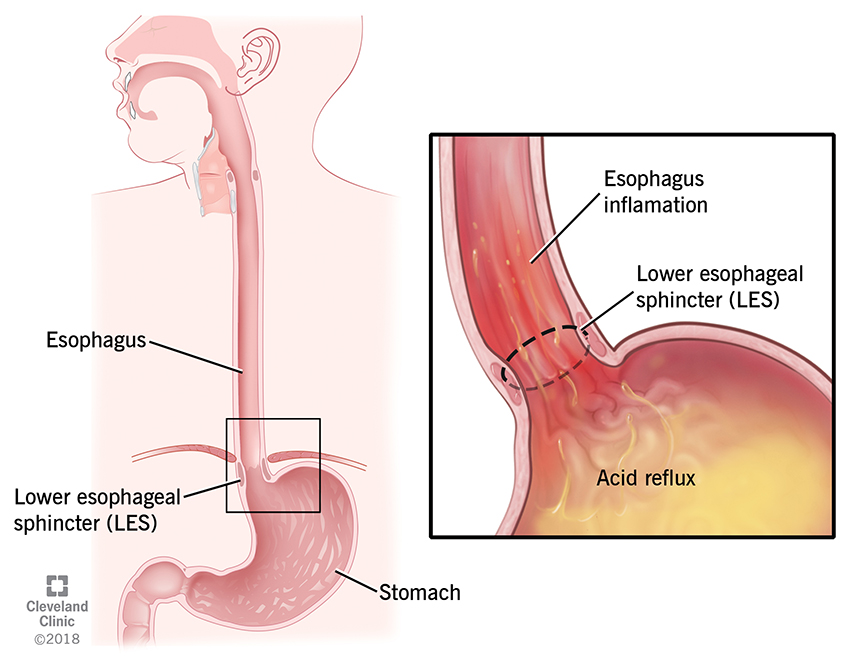
Let’s start by breaking down what GERD really means. The prefix -gastro stands for stomach, -esophageal means esophagus (the pipe leading food from your mouth to your stomach), and reflux is the burning or eroding of the esophagus. As we put these prefixes together, we can conclude that stomach acid backs up into the esophagus which causes burning and erosion of the esophageal tissues.
3 Types of GERD
The 3 types of Gastroesophageal Reflux Disease are non-erosive, erosive, and Barrett’s.
- Non-erosive is the most common type of GERD and patients are seen with characteristic symptoms without visible injury to the esophageal mucus.
- Patients with erosive GERD on the other hand have severe reflux determined by erosion or ulceration of the esophagus known as mucosal breakage.
- Barrett’s esophagus is a precancerous condition in which a patient’s esophageal lining suffers damage due to acid reflux causing thickening and inflammation of the esophagus.
How do I know if I have GERD?
Symptoms of Gastroesophageal Reflux Disease include heartburn, regurgitation, dysphagia or difficulty swallowing, and dyspepsia or epigastric discomfort. This can cause bloating, early satiety, nausea and belching. To prevent dyspepsia, reduce dietary fat intake and eat smaller, more frequent meals.
What are the causes GERD?
There are several etiologies or causes of GERD, however in this post we will be focusing on six:
- Lower esophageal sphincter tone
- The esophageal sphincter is a bundle of muscles at the top of the stomach or button of the food pipe. This bundle has a baseline for tone or tightness and this may be caused by smoking, alcohol, or caffeine. When the esophageal sphincter tone is low, this creates an issue as muscle does not clamp down causing irritation and burning from acidic backwash.
- Hiatal Hernia
- An outpouching of a portion of the stomach into the chest through the esophageal hiatus of the diaphragm. This may cause heartburn, regurgitation, or epigastric discomfort which are all symptoms of GERD (2).
- Some nutrition recommendations to help relieve these symptoms include smaller and more frequent meals, weight reduction, and possible surgery (2).

- Overproduction of hydrochloric acid
- Hydrochloric acid or HCl is acidic gastric juice produced in the stomach by parietal cells and the role of HCl is to break down food. Parietal cells produce acid based on the presence of food in the stomach which is stimulated by non-steroidal anti-inflammatory drugs (NSAIDS), alcohol, and smoking.
- Underproduction of hydrochloric acid
- Nutrients such as zinc, B vitamins, and iron are essential for maintenance of HCl production so if hydrochloric acid levels are low, this may lead to decreased or impaired absorption of these nutrients.
- A type of bacteria known as H. pylori often causes stomach ulcers and if this infection is left untreated it could be a major risk factor for low stomach acid.

- Changes in gastric pH
- Low pH of 1-3 is normal and desirable (6).
- High pH of 3-5 is abnormal and may present symptoms of GERD (6).
- High intragastric pressure
- When pressure within the stomach is higher than within the food pipe the stomach content can start pushing upstream into the esophagus causing reflux.
- Factors that can increase stomach pressure include pregnancy, obesity, large meals, and gastroparesis or delayed gastric emptying.
Treatment Medications
- Antacids
- Used for treatment of mild symptoms as antacids neutralize gastric fluid provide immediate relief. They decrease the activation of pepsinogen which breaks down proteins in food during digestion and should be taken after meals and at bedtime.
- H2-Receptor Antagonists (H2RA) or H2 Blockers
- Used for mild to moderate GERD. This medication blocks histamine at the H2 receptor site of acid producing cells which reduces the amount of stomach acid released in the stomach lining, therefore reducing symptoms.
- Proton Pump Inhibitors (PPIs)
- Used for moderate to severe and healing of erosive esophagitis. PPIs block gastric acid secretion by inhibiting gastric parietal cells similar to H2 blockers.
What may happen if left untreated?
- Esophagitis is irritation of the cells lining your esophagus due to exposure to the HCl. These cells may change their structure in an effort to protect themselves. Over time these changes can lead to the development of esophageal cancer (1).
- Severe esophagitis may result in extensive erosion, ulceration, and narrowing of the esophagus (1).
- Barrett’s esophagus is the conversion from one cell type to another in the esophagus as a result of acid exposure leading to esophageal cancer (1).
- Chronic esophageal inflammation from repeated acid exposure may lead to scarring or the development of peptic strictures (1).
- Odynophagia or painful swallowing (1).
Medical Nutritional Therapy
- Avoid large, high-fat meals and decrease greasy foods
- Avoid eating 2-3 hours before lying down
- Avoid carminatives: chocolate, mint, tomatoes
- Avoid caffeine
- Avoid alcohol
- Avoid acidic and highly spiced foods
- Consume a well-balanced diet with adequate fiber
- Smaller, frequent meals
Lifestyle Recommendations
- The two most common risk factors forGERD are alcohol and tobacco. It is recommended to quit smoking, avoid secondhand smoke, and stop the consumption of alcoholic beverages.
- Stress can affect many aspects of our lives including our health therefore reducing overall stress may help in reducing symptoms of GERD.
- Laying down after meals is not recommended as it may cause regurgitation of gastric acid and if patients suffer from reflux episodes at night, they should elevate their head of bed by 6-8 inches.
- Small frequent meals are recommended therefore modifying eating times to keep the reflux under control is ideal.
- Weight loss is a final lifestyle recommendation that should not be attempted without consulting a dietitian.
Supplements for GERD
Gastroesophageal reflux disease (GERD) symptoms can often be managed with the help of certain supplements. Here are a few that are commonly suggested:
- Melatonin: Many patients with GERD suffer from sleep disturbances. Studies suggest that it may have a protective effect against GERD. Melatonin supplements may help improve sleep quality and reduce symptoms of acid reflux.
- High Quality Melatonin in the right / lower dose is known to be most effective
- SHOP HIGH QUALITY MELATONIN HERE
- Probiotics: Probiotics are essential for healthy gut microbiome. They help maintain a balanced environment in the digestive tract and help to reduce symptoms of GERD. Probiotics are available in supplement form or can be obtained from fermented foods like yogurt and sauerkraut.
- Deglycyrrhizinated Licorice (DGL): DGL is a form of licorice where the compound glycyrrhizin which is know to increase blood pressure and other potential side effects, has been removed, making DGL safe. DGL helps soothe and protect the lining of the esophagus and stomach, providing relief from symptoms.
- L-Glutamine: L-Glutamine is an amino acid that plays a role in maintaining the health of the digestive tract lining. It is vitally important for the health of the GI tract as it repairs and reduces inflammation in the esophagus.
- Ginger: Ginger has anti-inflammatory properties and may help with digestion. It can be consumed as a supplement or in the form of ginger tea.
- Aloe Vera: Aloe vera may have anti-inflammatory effects and can be soothing to the digestive tract. However, its use for GERD is controversial, and it’s essential to use a form specifically designed for internal consumption.
- Magnesium: Some individuals with GERD may have low magnesium levels. Magnesium supplements may be considered under the guidance of a healthcare professional. Chelated for is best for GERD.
- Betaine HCL: Betaine HCL is believed to provide additional stomach acid, which may aid in the digestion of food. For individuals with insufficient stomach acid production, Betaine HCL might help improve the breakdown of proteins and enhance overall digestion as some people are underproduces of stomach acid. Betaine Hydrochloride (HCL) is a supplement that contains hydrochloric acid, a component naturally made by the stomach to aid in digestion and absorption of nutrients. If you suspect that you are making suboptimal lives of stomach acid Betaine HCL and resolve your symptoms for good.
Here is a simple way to determine if you are laking stomach acid. Take 1/2 to 1 teaspoon of baking soda, dilute it in 4 oz of water and drink it.
- if you feel worse –> this means that Betaine HCL is suitable for you.
- if you feel better —> this means that you have too much acid in your stomach and Betaine HCL will not help. In this case ace use, DGL, Aloe Vera or Ginger and L – Glutamine which can be combined with other supplements.
- Take on bill from Betaine HCL before your meal.
- SHOP HIGH QUALITY BATAINE HCL HERE
If you suffer from stomach ulcers such as peptic ulcers, gastritis, or other stomach-related issues, Betaine HCL is not appropriate for you.
Citations
- Clarrett DM, Hachem C. Gastroesophageal Reflux Disease (GERD). Mo Med. 2018 May-Jun;115(3):214-218. PMID: 30228725; PMCID: PMC6140167.
- Hiatal hernia Symptoms & Treatment | Aurora Health Care. (n.d.). Aurora Health Care. https://www.aurorahealthcare.org/services/gastroenterology-colorectal-surgery/hiatus-hernia-hiatal-hernia#:~:text=A%20hiatal%20or%20hiatus%20hernia,an%20opening%20in%20the%20diaphragm.
- Lipski, E. (2000). Digestive wellness. Keats Publishing.
- Lipski, L. (2000). Gut Related Disorders Track 2 Module 1: GI Part 1 [PowerPoint slides]. Integrative and Functional Nutrition Academy. https://acrobat.adobe.com/link/track?uri=urn:aaid:scds:US:13669dbf-dbdb-4a85-a88f-8ce28526530c
- Professional, C. C. M. (n.d.). Acid Reflux & GERD. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/17019-acid-reflux-gerd
- What is pH? | US EPA. (2023, November 6). US EPA. https://www.epa.gov/goldkingmine/what-ph
